Innovative Technologies
Innovative Technologies
Nihon Kohden has developed innovative and unique technologies that contribute to progress in medical care. We boldly take on new challenges, maintaining a keen eye for detail as we keep in mind the spirit of the founder.

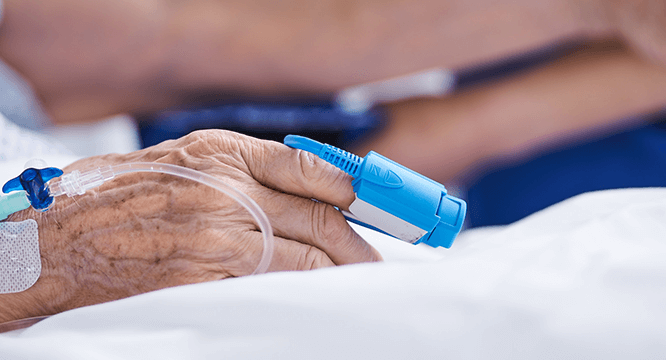
The Pulse Oximeter is a device that continuously and non-invasively monitors the level of oxygen in patients’ bloodstream. The principle of pulse oximetry was invented by Dr. Takuo Aoyagi, an engineer at Nihon Kohden, in 1972.

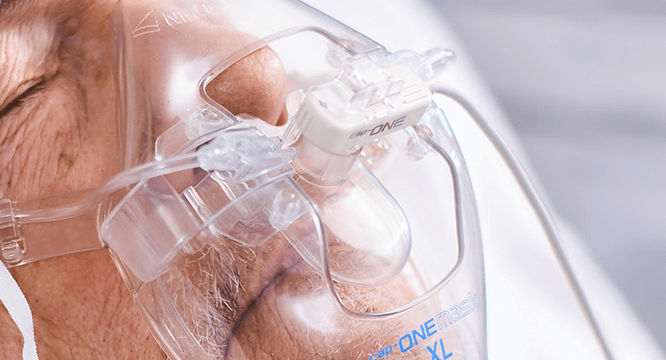
cap-ONE is Nihon Kohden's unique mainstream CO2 sensor for both intubated and non-intubated patients. The ultra compact sensor and unique adapter provide accurate measurements and reduce the burden on the patients. cap-ONE overcomes the disadvantages and maintains all the advantages of mainstream sensor for optimal capnography.

esCCO provides cardiac output information only using common vital sign parameters of ECG, SpO2 and blood pressure, requiring no additional sensors or special trainings. Hemodynamic trend monitoring will be available with esCCO for all care levels, not only during major surgeries but also in lower-risk procedures for high-risk patients showing a higher chance of bleeding or any hemodynamic stress. Also, esCCO can be a reliable index during fluid administration in various clinical settings. Adding esCCO to the conventional patient monitoring may lead to optimization of fluid management, decreased risk of complications and eventually to better outcome including reduced length of stay.


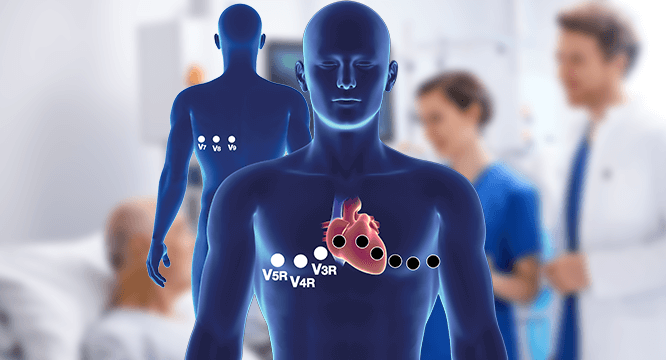
The most common ECG exam is the standard 12-lead ECG. It is simple to measure, has a low burden on the body, and observing the heart from these 12 directions provides a lot of information with a wide range of clinical applications. However, some areas, especially pathological changes in the right ventricle and the posterior wall, cannot be observed from the 12-lead ECG.

iNIBP is Nihon Kohden's non-invasive blood pressure measurement algorithm using inflation technology. iNIBP completes the measurement while inflating a cuff.


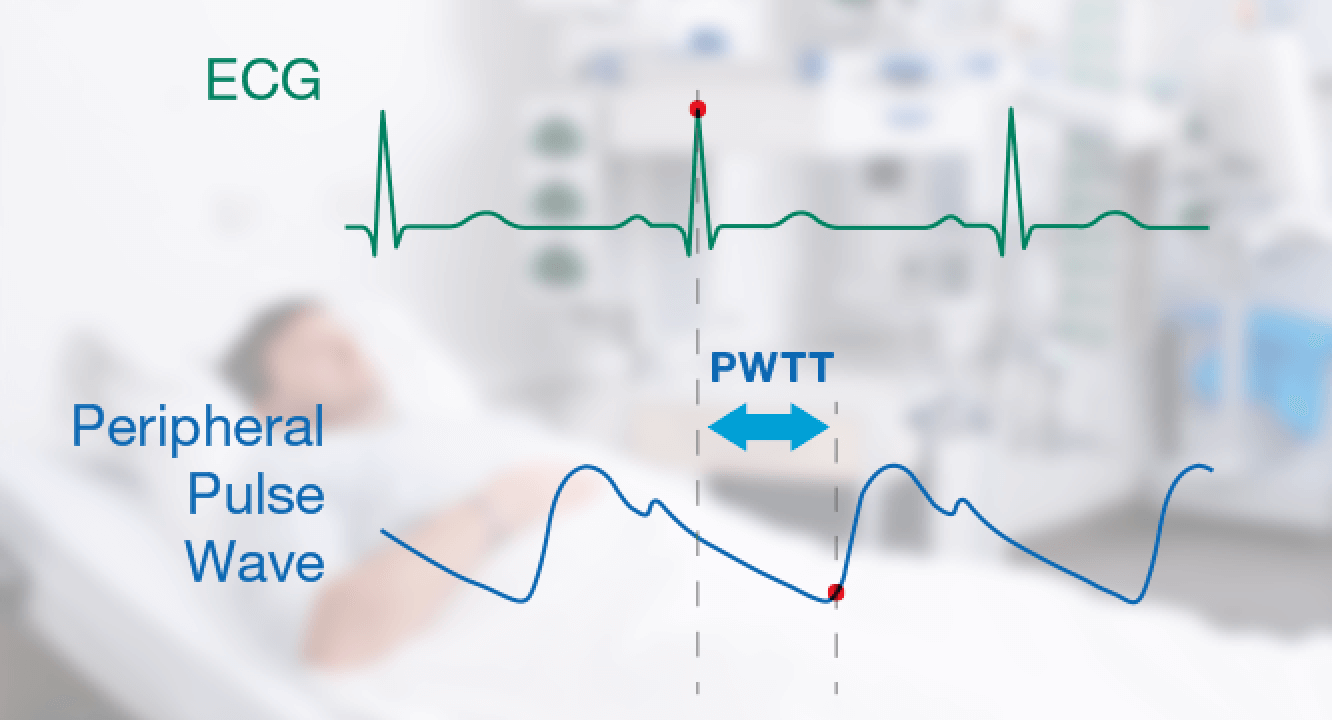
PWTT (Pulse Wave Transit Time) is obtained by the pulse oximetry and ECG-signals from each cycle of the ECG and peripheral pulse wave. If PWTT exceeds the threshold during periodic NIBP measurement, it triggers NIBP measurement. This increases the chance to detect sudden change in blood pressure between periodic NIBP measurements. Together with periodic NIBP measurement, this can provide more complete blood pressure monitoring with no additional sensors or modules required.
Nihon Kohden offers the Gentle Lung® package for the NKV-550/440 ventilator, which consists of four convenient tools for clinicians to practice lung protective ventilation.

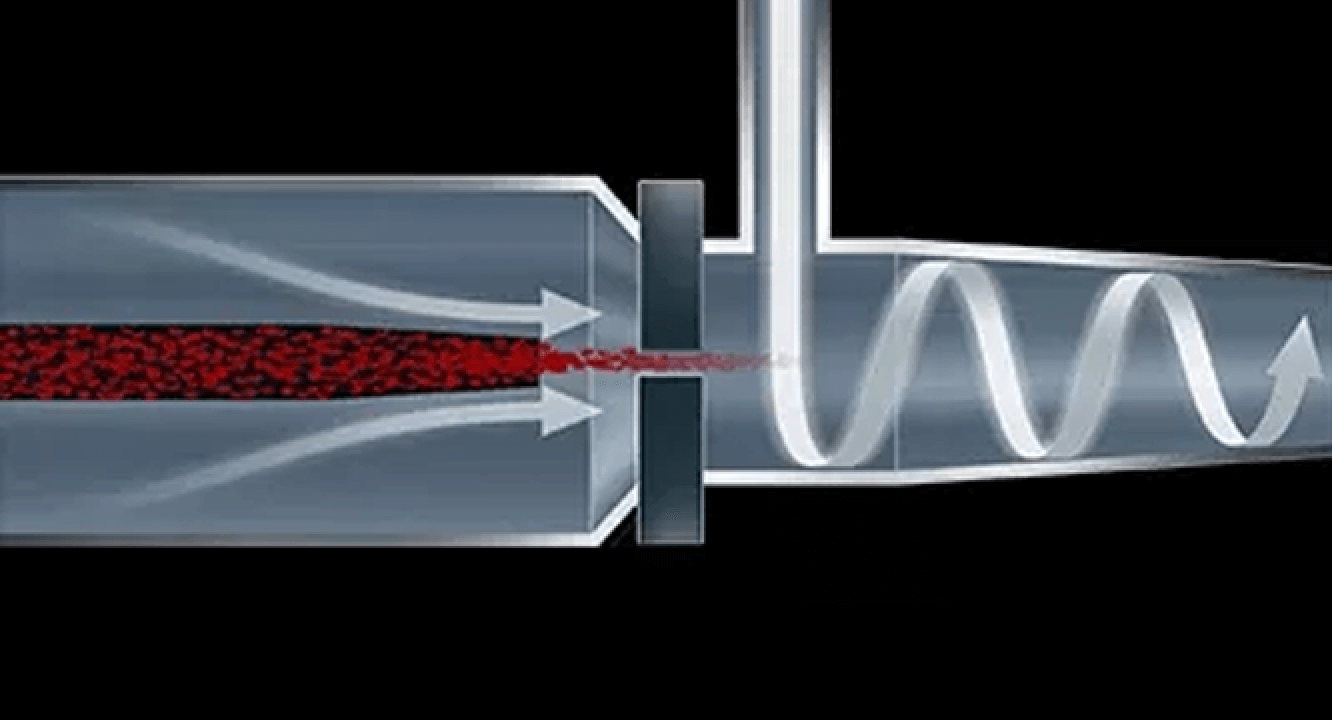
The DynaHelix Flow technology perfectly aligns WBC, RBC and PLT cells for high impedance counting precision using advanced hydrodynamic-focused sheath flow before passing through the aperture.

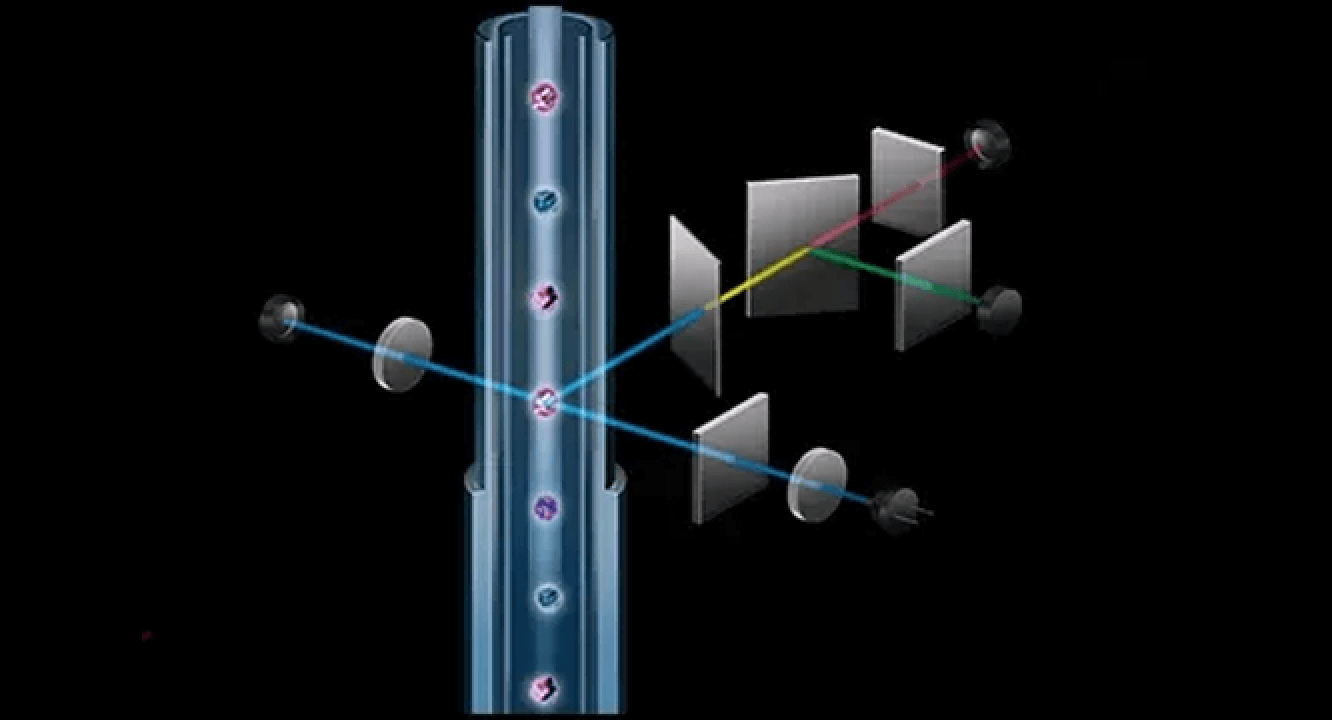
Integrated Technology with Small Laser Optics, Optimized Reagents, and New Analysis Algorithms.
DynaScatter Laser optical technology analyzes and differentiates WBSs in near-native state.

CiRHEX* Technology provides ESR results highly correlated with the Westergren method in 2 minutes. It uses the HCT value and MCV value from CBC measurement and the RBC aggregation phenomenon.