The ICU is changing: Why advanced non-invasive haemodynamic monitoring is gaining ground – Featuring esCCO by Nihon Kohden.
23. July 2025
In the high-stakes environment of intensive care, clinicians rely heavily on haemodynamic monitoring to guide life-saving decisions. But how are those monitoring methods evolving? And what role will non-invasive technologies play in the future of critical care?
To better understand current practices and preferences, we conducted a professional survey targeting ICU clinicians, physicians, and biomedical experts. The insights reveal a clear trend toward non-invasive haemodynamic monitoring—with a growing trust in solutions like esCCO by Nihon Kohden.
Survey Highlights
We asked five targeted questions focused on haemodynamic monitoring practices, preferences, and challenges. Here’s what we learned:
Haemodynamic monitoring is a daily essential
100% of respondents reported using haemodynamic monitoring either always or frequently. This reaffirms its importance in managing critically ill patients, particularly when it comes to fluid responsiveness, cardiac output, and perfusion monitoring.
Methods are shifting toward non-invasive technologies
While invasive and minimally invasive tools are still in use, many respondents cited non-invasive methods like bioimpedance, ultrasound, and esCCO by Nihon Kohden as part of their routine.
The data signals a growing trust in non-invasive solutions, particularly when they deliver reliable and continuous data without compromising patient safety.
Invasive monitoring comes with challenges
The primary concerns around invasive methods included:
- Risk of infection or complications
- High resource demand (time, training, equipment)
- Impact on workflow
These pain points open the door for smarter, faster, and safer alternatives—especially in high-volume ICU settings.
Non-invasive = Reliable in the eyes of clinicians
A combined majority rated non-invasive technologies as:
- “Highly reliable – a strong alternative to invasive methods”
- “Generally reliable – useful in most clinical settings”
This reflects a maturing confidence in modern non-invasive platforms, and a readiness to move away from catheters and lines—when the data supports it.
Introducing esCCO by Nihon Kohden: Non-invasive. Continuous. Reliable.
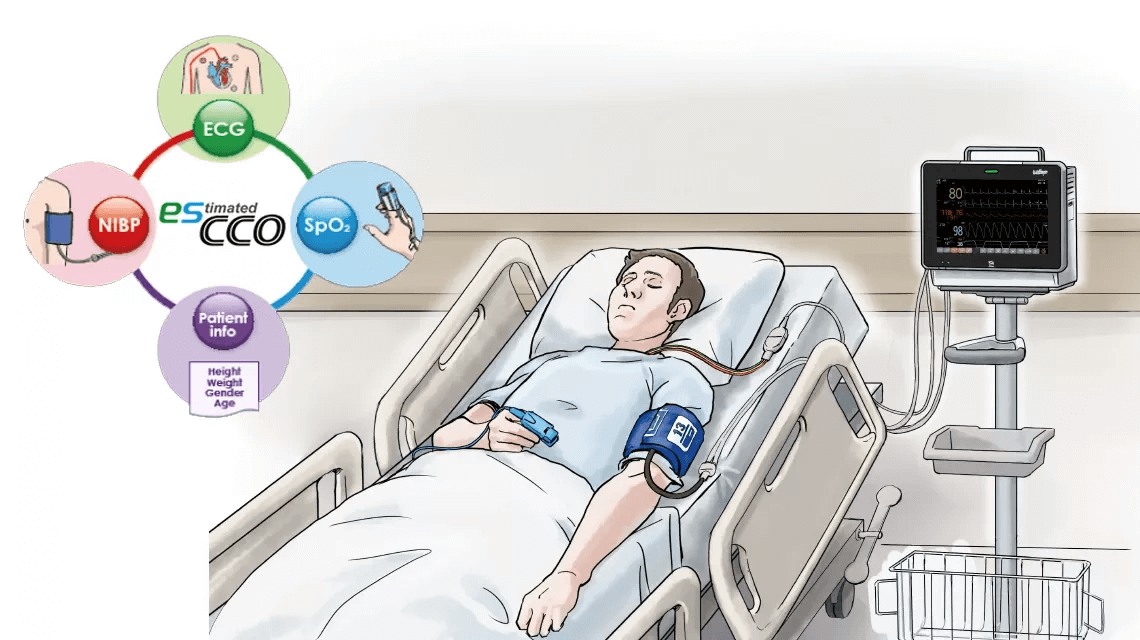
esCCO (estimated Continuous Cardiac Output) offers real-time cardiac output and stroke volume measurements—without requiring any invasive catheters or calibration procedures.
What makes esCCO unique?
- No arterial line required
- Real-time, beat-to-beat measurement
- Works with standard ECG, SpO₂, and NIBP monitoring
- Improved patient safety and comfort
- Faster setup and streamlined workflows
With esCCO, clinicians get the data they need to make fast, informed decisions—while minimizing patient risk and system burden.
The takeaway message: A future-ready approach to haemodynamics
Our survey confirms a paradigm shift: ICU clinicians are increasingly prioritizing efficiency, safety, and non-invasive accuracy.
Solutions like esCCO by Nihon Kohden directly address the concerns voiced by today’s healthcare teams. They offer a clinically validated, cost-effective, and scalable solution for modern critical care environments.
Non-invasive doesn’t mean less capable. With esCCO, it means more efficient, more scalable, and more aligned with the future of ICU medicine.